is a life-threatening complication accompanied by high mortality rates in cases of late diagnosis and inadequate treatment. Mediastinitis is a common complication of infectious diseases, but still the majority of mediastinitis cases in the world are the consequence of cardiac surgical interventions. Despite modern advances in antimicrobial therapy, immunotherapy and surgical technologies, purulent-septic complications after median sternotomy are a serious problem in modern health care. Treatment of mediastinitis as a form of generalized purulent infection includes long-term intensive care and complex set of surgical interventions. In addition, the duration of hospital treatment and cost increase. This is explained by additional cost of diagnosis for this complication and a full range of intensive care accompanying a series of reoperation. The cost of treatment of mediastinitis after cardiac surgery is comparable to that of acute renal failure.
Development of acute postoperative mediastinitis is often unpredictable. Treatment is difficult as well because of the anatomical features of the mediastinum due to poor blood supply and the tendency to form blind pockets (dead space). Devascularized sternum, suture and prosthetic materials further complicate the conditions of treatment. Septic-purulent nosocomial infection is one of the most important problems of modern health care. The urgency of this problem is primarily determined by the spread of these infections and significant social and economic losses caused by them. Among the factors determining the growth trend of nosocomial infections are widespread use of invasive diagnostic and therapeutic manipulation, spread of hospital antibi- otic resistance strains of microorganisms, and growing percentage of elderly people.
Along with the natural propagation mechanisms septic-purulent nosocomial infections, artificial mechanism of transmission of nosocomial infections associated with invasive diagnostic and therapeutic procedures has formed and does actively operate. Among the urgent tasks to combat nosocomial infection is maximum reduction in duration of hospital stay, without reducing the volume and quality of medical diagnostic and rehabilitative care.
This paper demonstrates literature analysis and also reviews the Center ’s little experience in treating patients of this category.
Most surgeons currently prefer longitudinal sternotomy as a universal surgical access in interventions on the heart with cardiopulmonary bypass. Despite modern advances in antimicrobial therapy, immunotherapy and surgical technologies, purulent-septic complications after median sternotomy, in particular the front mediastinitis, according to different authors, occur in 1-5% of all transsternal operations [Curtis JJet al., 2001]. Its development is often unpredictable. Treatment is difficult because of the anatomical features of the mediastinum characterized by poor blood supply and the tendency to form blind pockets (dead spaces).
Devascularized sternum, suture and prosthetic materials additionally complicate the conditions of treatment. Mortality in standard therapy is still high 14-23%, and without it makes 100% [El Oakley R M et al., 1997; Upton A et al., 2005].
Braxton JH et al demonstrated in their work that during coronary bypass surgery in 36078 patients, mediastinitis occurred in 418 (1.16%). Mortality rate was significantly higher in the group where mediastinitis complicated postoperative course, than without it - 11.15 per 100 person / years and 3.81 per 100 person / years, respectively, (P <0.001). In the late period, 6 months after the operation, these figures were 5.7 and 2.66 deaths per 100 person/ years respectively, (P <0.001) [Braxton JH et al., 2004]. According to others, the development of mediastinitis also negatively affects not only the immediate survival of patients, but also long-term results of treatment. According to Milano CA mortality rate in patients with mediastinitis within the first 90 days after surgery was 11.8%, in the group with-out mediastinitis it was 5.5%. The comparable figure for the period from 1 to 2 years after surgery was 8.1% and 2.3% [Milano CA, 1995].
In their work Finkelstein R et al (2005) provided less optimistic data: surgical site infections in cardiac surgical patients occurred in 10.4%. At the same time, the incidence of mediastinitis remains low and makes 3.25% - 1.48%.
Colleagues from the Vishnevsky Central Military Hospital present data on surgical treatment of 3259 patients, of whom 49 patients (1.5%) developed mediastinitis. Mortality was in 8.3% (4) patients, the cause of death was sepsis (1 patient), repeated transmural myocardial infarction (2) and a massive stroke in the left hemisphere of the brain (1) [Kohan EP, Alexandrov AS, 2011]. Yekaterinburg №1 Regional Center for Cardio-vascular Surgery reports on the treatment results of 535 patients who underwent various cardiopulmonary bypass surgeries. In this series of observations front mediastinitis was diagnosed in 28 (5.2%) patients [Abboud CS et al., 2004].
Mediastinitis manifestations can vary from subacute up to critical. A typical course of postoperative mediastinitis is accompanied by fever, tachycardia and development of local signs of wound infection in the sternotomy access area. In 2/3 cases these symptoms occur within the first 14 days after surgery. In a later manifestation of infection clinical signs the major complications are chest pain that increases with time, and progressive hyperemia in postoperative suture. The weakening of systolic heart sounds on auscultation precordial area (Ham- man’s sign) is a reason for possible mediastinitis, but a negative result does not rule out the development of this complication. Local signs of sternum infection may be among the earliest, however they may occur when the diagnosis of mediastinitis is already beyond doubt and confirmed by other methods. There may be all or partial symptoms: pain in the sternum, the instability of the sternum, presence of local or widespread soft tissue infection, and wound discharge. If they are accompanied by signs of sepsis, most likely, it points to the development of deep infection and mediastinitis.
According Cardenas-Malta KR et al the main clinical signs of descending necrotizing mediastinitis were pyrexia (100%), pain in the surgical wound (85%), intermittent fever persists for more than 5-7 days in the early postoperative period (73%), purulent discharge from the wound (60%), dysphagia (80%), dyspnea (80%), chest pain (60%), orthopnea (40%), and tachycardia (20%). In 80% of cases lesion of mediastinum resulted from odontogenic infection [Cardenas-Malta KR, 2005; Kohan EP, Alexandrov AS, 2011].
Diagnostics of mediastinitis is based on intensive dynamic X-ray study [Ho MW et al., 2005], but computed tomography still provides the most detailed information on the prevalence of the process [Scaglione Met al., 2005]. Computed tomography is most informative to identify levels of liquid and gas in the mediastinum. This method allows diagnosing postoperative sternum dehiscence and identifying small accumulation of fluid in the retrosternal space. Computed tomography can be used in the postoperative period to monitor local processes in the mediastinum. After 2 weeks of postoperative period CT sensitivity and specificity is approximately 100% [Jolles H et al., 1996]. Signs of mediastinitis detected by computed tomography are (percent of occurrence indicated):
- increase in the mediastinum size (100%)
- local accumulation of fluid in the mediastinum (55%)
- free gas in the mediastinum (57.5%)
- increase in mediastinal lymph nodes (35%)
- pericardial fluid (27.5%) and pleural cavities (85%)
- pulmonary infiltration (35%)
- sternal incision dehiscence (40%)
- mediastinal pleura fistula (2.5%)
Signs of mediastinitis, detected by CT, are divided by some authors into direct (local accumulation of fluid in the mediastinum and pneumomediastinum) and secondary, the presence of which can be caused also by other factors (tissue swelling mediastinal lymphadenopathy, pleural effusion, pulmonary pathology and sternum). In up to 14 days the primary signs of mediastinitis are nonspecific (sensitivity 100%, specificity 33%). Their presence at a later date is a reliable sign of postoperative mediastinitis (sensitivity and specificity of 100%) [Jolles H et al., 1996]. Mediastinitis diagnosis by CT can be much earlier than the changes will be visible on conventional multipositional radiographs [Takanami I, Takeuchi K, 2001; Mihos P et al., 2004]. In this case, spiral computed tomography has an advantage [Pinto A et al., 2003]. The widespread use of CT also makes it possible to quickly diagnose the inflammatory process in the neck and mediastinum and perform urgent drainage of all identified purulent foci [Papalia E et al., 2001]. The most important laboratory diagnostic technique is culturing the wound for the pathogen and antibiotic susceptibility.
Of the main risk factors for mediastinitis most authors highlight [El Oakley RM, Wright JE, 1996; ATMI1999; Gummert JF et al. 2002; Abboud CS et al.2004; Belov VA, 2005; Imamaki M et al. 2005; Lepelletier D et al. 2005; Sjogren J et al. 2005; Upton A et al. 2005; Reyna GC et al. 2006; Kohan EP, Alexsandrov A.S 2011]:
- obesity more than 20% of ideal body weight
- operation of bilateral coronary artery bypass grafting
- diabetes
- the urgency of the operation
- the presence of extrinsic compression of the heart
- shock in the postoperative period, especially if there has been a massive blood transfusion
- a long period of time and cardiopulmonary bypass surgery
- reoperation
- postoperative pneumonia
- urinary tract infections
- conducting IABP
- postoperative dehiscence (sternotomy) wounds
- technical features of the operation (overuse of electrocoagulation, processing of bone cut with paraffin, performance of paramedical sternotomy)
The need for a tracheostomy after coronary bypass surgery also increases the incidence of mediastinitis from 0.7% to 8.6% (P <0.001) and lethality from 5, 2% to 24.7% (P <0.001), but did not affect the duration of hospitalization [Curtis JJ et al. 2001].
According to American colleagues, mediastinitis most often occurs after bypass surgery (coronary artery bypass, mammary coronary artery bypass grafting), the frequency of complications in most major centers is 1-2%.The risk of mediastinitis after heart transplantation is significantly higher [Baldwin RT et al., 1992]. According to Walkes JC et al (2002), the incidence of postoperative mediastinitis is 2 times higher for the bypass using the two internal thoracic arteries as compared with the one, thus making 4.4% [Weinzweig N, Yetman R, 1995]. Pos-sible development of mediastinitis due to infected graft transplantation is reported [Burket JS et al. 1999].
El Oakley RM classified post-sternotomy medi-astinitis into five types:
Type 1 - develops within the first 2 weeks after surgery in the absence of factors risk Type 2 - develops on the 2nd-6th weeks in the absence of risk factors тУРе 3 - mediastinitis types I and II in the presence of one or more risk factors: diabetes, obesity, use of immunosuppressive or hormone replacement therapy тУРе 4 - mediastinitis I, II, or type III after one or more attempts of ineffective treatment; Type 5 - develops the first time in more than 6 weeks after surgery [El Oakley RM, Wright JE, 1996].
When assessing mediastinitis other authors classify poststernotomy mediastinitis as sternal dehiscence without infection and with infection, with the latter being subdivided into several subtypes, including restriction of infection to soft tissue, sternal osteomyelitis, and retrosternal infection [El Oakley RM, Wright JE, 1996; Thomas J, Kouchoukos N, 2001; Reyna GC et al., 2006]: type 1 usually occurs within 3-5 days of the postopera-tive period and is characterized by the presence of uninfected serous-hemorrhagic exudate and the absence of osteomyelitis of the sternum, type 2 postoperative mediastinitis is marked by later development, from 1 to 3 weeks of the postoperative period with necrosis nidi of mediastinum soft tissues, without osteomyelitis of the sternum and ribs and/or rib cartilage, and type 3 mediastinitis, which develops after 1 month after surgery, is marked by chronic osteomyelitis, necrosis of the bone, rib cartilage and mediastinum soft tissues, resulting in “dead” spaces and “blind” pockets.
Classification of transsternal access complications Sternum dehiscence - postoperative wound dehiscence in the absence of clinical signs of infection or positive culture. Sternotomy wound infection - proven clinical or microbiological evidence of presternal tissues infection, as well as sternum osteomyelitis. Surficial infection - infection affects thoracic tissue (“anterior mediastinitis”). Deep wound infection or mediastinitis - sternum osteomyelitis with or without involvement of the deep mediastinal structures.
Currently, most of the authors adhere to active surgical approach to all mediastinitis patients, regardless of the clinical course, as without surgical rehabilitation mediastinal mortality rate ranges from 70 to 100% [Panteleev SM, 1999; Finkelstein R et al., 2005]. However, some authors believe that it is possible the effective reversal of symptoms of poststernotomy mediastinitis using closed drainage of purulent nidi with Redon catheter [Kirsch M et al., 2001]. In most cases, the best strategy is determined individually, in accordance with the duration of infection, degree of involvement in the inflammatory process of the mediastinum and the state of mediastinal structures, and also by drawing on the surgeon’s experience.
According to other authors, widespread presence of purulent-necrotic process inevitably requires repeated intervention by “open” management the of the wound for a few days, phase-based necrectomies and subsequent application of secondary sutures and the use of plastic closure of the defect, mostly by muscle flap [Robicsek F, 2000].
Usually after debridement, eradication of necrotic tissues with subsequent irrigation therapy during intensive treatment is sufficient (mediastinitis types I and II). In some cases, open management of mediastinal wound has a negative impact on the mechanics of breathing and creates conditions for the development of erosive bleeding. Therefore, based on clinical data and intraoperative findings, the operating surgeon can make a choice between either the primary surgical wound suturing, which is possible in rare cases of mediastinitis, or the use a combination of large diameter drainage pipes and irrigation devices for multi-day washing of mediastinum with antibiotics and antiseptics. In non-purulent poststernotomy mediastinitis reoperation with sanitation, drainage and sternum stabilization and suturing the wound is deemed necessary [Robicsek F, 2000].
In the treatment of postoperative type IV and V mediastinitis the safest and most effective treatment strategy is extensive mediastinal tissue excision followed by delayed plastic repair with muscle flap or strand of the greater omentum. The choice of plastic method is determined by the plastic surgeon’s experience and preferences, as well as the nature of the patient’s condition. Considering the omentum’s more active role in the implementation of local immunity and in angiogenesis, in some cases mediastinum omentoplasty has an advantage over muscle flap [Weinzweig N, Yetman R, 1995].
According to Russian authors mediastinitis treated by open method does not give promising results. Application of this method is accompanied by respiratory failure due to disorder of the thorax carcass integrity, patient’s discomfort from injury, and the risk of erosive bleeding. With this method of treatment the average duration of patients’ hospitalization is 90-120 days. Mortality in open management is 33.3%. In the presence of “closed” wound management using continuous flow dialysis, treatment of mediastinitis was conducted in accordance with the plan including resternotomy, sanitation and drainage of the mediastinum with two tubes followed by constant irrigation of the cavity with disinfectants and active content aspiration. Duration of drainage of the mediastinum is 8-10 days. Treatment of mediastinitis closed method using a flow dialysis causes no big failure and respiratory discomfort for the patient. However, this method has disadvantages resulting from grafting of antiseptic solution between the drainage tube, and, as a result, uneven irrigation of the mediastinum, development of purulent leakage, leading to a potential relapse of the infection. The presence of the drainage system limits the motor activity of the patient, moreover; wound irrigation requires a large amount of fluids (about 4 liters).The average duration of stay of patients in hospital is 17-28 days. Mortality in the “closed” management of patients is 19%. Omento- mediastinopexy method, which has recently been widely used in the treatment of anterior mediastinitis, is simple and available to perform for any surgeon. Blind suture of the wound does not cause discomfort to the patient, it allows the patient to be mobile and active, and reduces hospital stay up to 12-14 days. Mortality in this method of treatment is close to zero. All patients showed a good result [Kohan EP, Alexandrov AS, 2011; Netscher DT et al., 2001; Schroeyers P et al., 2001]. Thus, the ad-vantage of the omentoplasty method over other methods of treatment of postoperative mediastinitis is undeniable. The advantage is due to its high ef-fectiveness, the method allows achieving complete recovery for this group of severely ill patients, and in contrast to other methods of treatment, is not ac-companied by mortality. This reduces the length of stay of patients in hospital, which has a significant economic effect.
Omentoplasty is not indicated if gastroepiploic artery has been used in bypass surgery. If internal thoracic artery or internal mammary gland was used in the bypass, it is impractical to perform plastic repair with rectus abdominis muscle flap. In these situations plastic flap of the greater pectoral muscle should be preferred.
According to Belov VA (2005) surgical strategy with mediastinitis is different, but there is general agreement on three principles:
• The infectious process must be controlled in the earliest possible time
• All cases of mediastinitis require adequate drainage
• Failsafe stabilization of the sternum is necessary
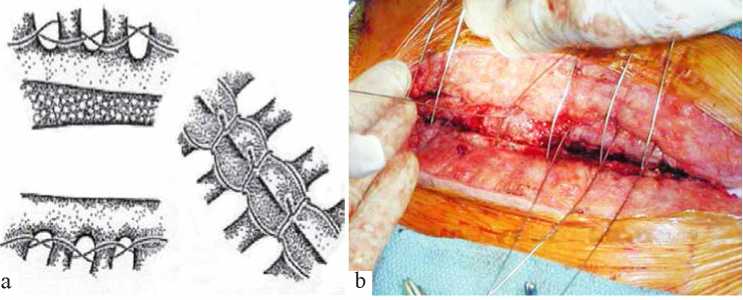
Resternotomy, mediastinal irrigation with an antibiotic solution without removing the drainage system, and stabilization of the flexible edges of the sternum are performed in mediastinitis type 1. In the presence of osteoporosis or breakage of the sternum, intertwined stabilization technique of the sternum is performed. In such cases, parasternal continuous suture is used. During this procedure, the wire is held in parallel with the suture on both sides of the sternum. Every suture starts at the lowest sternocostal joint and reaches, alternating intercostal space in the anterior-posterior direction, the second sternocostal joint. The suture is applied in two directions and then tightened. Seven or eight transverse separate sutures are subsequently ap-plied on the sternum in tight adjustment. Particular attention is paid to the location of the longitudinal seams of the sternum suture in order to avoid damage to the internal thoracic artery (Fig. 1). In some cases, if the cut is off the center of the sternum and costal cartilages are broken off, on the current side the initial part of a continuous suture is applied in the cranial direction not towards intercostal spaces, but through the costal cartilage.
 |
 |
In the second type of postoperative mediastinitis, in addition to surgical approach similar to that in type 1mediastinitis, surgical treatment of anterior mediastinum (sanitation) of all necrotic tissue (bone, cartilage, soft tissue) is used. Plastic repair using the greater pectoral muscle flaps and the omentum is recommended.
In the third type of mediastinitis, which develops after 1 month after surgery, chronic osteomyelitis, bone necrosis and cartilage mediastinal soft tissue with the formation of dead spaces are observed. Surgical approach requires extensive excision of necrotic tissue, up to a full sternectomy, and subsequent open management until full wound cleansing and subsequent thoracoplasty. All patients participating in the study, whose postoperative period got complicated by the development of acute anterior mediastinitis, underwent surgery after diagnosis in a matter of urgency. Closed technique based on the above principles was used, yielding good immediate results. In 10 cases, the sternum was fixed using parasternal reinforcing suture. This technique of management and surgical tactics in acute anterior mediastinitis described above proved its efficiency and reliability.
Below is a brief experience in this category patient treatment at the Kaliningrad Federal Cardiovascular Surgery Center. From September 2012 to August 2014, in cardiac surgery department, 799 operations via median longitudinal sternotomy were performed. Anterior mediastinitis developed in 7 (0.8%) patients, 16 (2%) patients suffered from postoperative wound dehiscence of the soft tissues without affecting the sternum. In these patients, as a rule, the treatment was not very challenging. After 5-7 day open wound management in the absence of discharge and the presence of the signs of wound cleansing, repeated suturing was performed 10-12 days later; after removal of secondary sutures the patients were discharged from the hospital.
In the development of mediastinitis we adhere to active surgical approach for all patients, regardless of the clinical course, because in accordance with literature data without surgical rehabilitation mediastinal mortality rate ranges 70 to 100% [Panteleev SM, 1999; Scott CH et al., 2001]. The most reliable signs of mediastinitis were wound pain, intermittent fever persisting over 5-7 days in the early postoperative period, purulent wound discharge and instability of the sternum in 7 patients (0.8%).
According to the laboratory research data, as a rule, inflammatory changes in the blood were detected in most operated patients, but this pattern can be misleading because of the general reaction of the organism to surgical trauma and cardiopulmonary bypass. In recent years, the number of erased clinical forms of mediastinitis manifested only one or two of these symptoms. This is due to the use of powerful modern antibiotics. Of great diagnostic importance is the Gram staining method of samples obtained from the wound discharge - the first stage of microbiological diagnostics, allowing for a mi-crobiological diagnosis and commencement of a rational empirical antibiotic therapy.
Computed tomography is the most informative in-strumental method of diagnostics that allows identifying levels of fluids and gas in the mediastinum. This method allows diagnosing the sternum dehiscence after surgery and identifying small accumulations of fluids in the retrosternal space. Transesophageal ultrasonic examination employing diagnostic fine needle biopsy of the mediastinum and subsequent microbiological analysis of the biopsy specimen can be used as a diagnostic method, clarifying the computed tomography data [Prasad VM et al., 2000; Fritscher-Ravens A et al., 2003].
In 7 (0.8%) patients of the El Okley RM and Wright JE classification, type I mediastinitis was diagnosed in 2 (0.2%) patients, III type in 3 (0.3%) and IV type in 2 (0,2%) patients. All patients with type I mediastinitis, two patients with type III and one with type IV underwent comparison of the sternum by the conventional method (using a separate 8-shaped wire sutures). In one patient Robicsek suture was used (Fig. 1) and in a patient with the most serious complications thoracic omentoplasty technique was used, employing greater pectoral muscles (a more detailed description of the patient is given below).
Patient D. 59 years was admitted to hospital in July, 2014. After a full follow-up examination primary she was diagnosed with ischemic heart disease. Stable cardiac angina of type III functional class. Post-infraction cardiosclerosis (posterior heart attack in May, 2013), hypertensive heart disease. Risk level III of cardiovascular complications. Complication: stage II A chronic congestive heart failure of type III functional class (New-York Heart Association). Concomitant: level III obesity. Type 2 insulin- dependent diabetes mellitus at the stage of sub-compensation. Diabetic foot, healed trophic ulcer of second toe of the left foot. Diabetic nephropathy, a stage of microalbuminuria, II class chronic kidney disease, chronic pancreatitis, chronic pancreatitis, hepatic steatosis.
Operation is performed: mammary coronary bypass of the left anterior interventricular artery. Early postoperative period was uneventful, on the second day after surgery the patient was transferred from intensive care ward in a general ward. Daily dressings were done, there were no signs of postoperative wound inflammation. However, 12 days after the operation turbid serous discharge from the upper corner of the wound appeared, hyperemia of skin edges. Dressings were continued using 10% hypertonic solution. Antibiotic therapy was introduced. Two days later, negative changes were observed as dehiscence of skin edges and increased discharge from the wound, the wound was affected in the soft tissues. According to computed tomography, sternal dehiscence reached 7 mm, there were signs of inflammation in the retrosternal space. The patient underwent reosteosynthesis of the sternum. It was fixed up by 5 wire 8-shaped sutures. After surgery, the patient experienced sudden cardiac arrest followed by resuscitation on the closed type giving a positive effect. On the third day after the operation purulent discharge the lower corner of the wound was observed again, the wound was throughout. Eruption of wire joints and fragmentation of the sternum were observed. A decision was made to continue with wound management using a vacuum bandage. Dressings were done once in every three days, cultures were repeatedly taken from the wound discharge for further identification of the pathogen and sensitivity to antibiotics. After bandaging for 7 times the wound was clean and actively granulating, and according to the bacteriological examination it did not show growth of pathogenic flora. Thoracic omentoplasty was performed and irrigation system set up. The first stage involved supramedian laparotomy. Greater omentum flap on feeding vessels was extracted. The flap was placed into the abdominal cavity. The post-sternotomy wound showed dehiscence. The sternum was debrided, mostly absent. The tissues of the anterior mediastinum exhibited granulation. No discharge. Resection of granulations followed, skin scar was excised, edges of the sternum reached active bleeding. Flaps of greater pectoral muscles on both sides were mobilized. The flap of the great omentum was moved to the anterior mediastinum and fixed to the tissues of the mediastinum with 10 single prolene sutures 5/0. Irrigation system for sanitation and 24F drainage was set up under the greater omentum. Thoracoplasty was performed using greater pectoral muscle flaps above the greater omentum with 5 U-shaped and continuous Etilon 2/0suture. Drainages were placed in the beds of the greater pectoral muscles on both sides. Layered suturing of wounds was performed. Operation stages are shown in Figure 2.
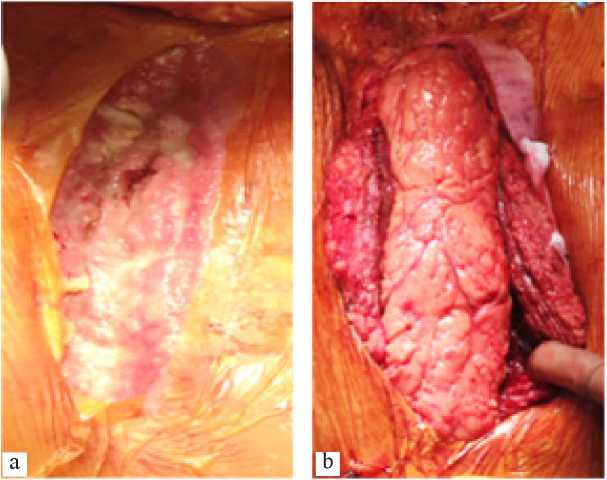 |
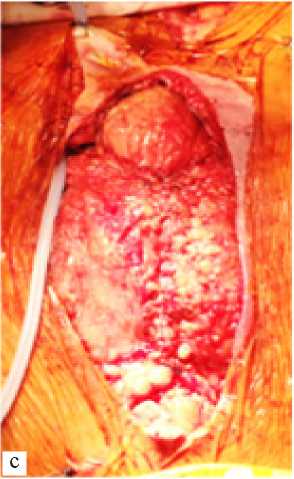 |
The wound irrigation required 200 ml of 0.2% aqueous solution of chlorhexidine per day, with the addition of 2 ml of a 10% Betadine solution for 5 days, under stringent control of incoming and outgoing volume the fluids. Subsequently, after removal of the drainage tube on the 12th day the patient was discharged from the Center. Consistent follow-up for 2 months revealed complete healing of the wound.
Treatment of postoperative sternal osteomyelitis is a serious challenge for thoracic surgery, because one-time rehabilitation of the infection area often does not lead to a positive result. Plastic techniques, as the final stage of treatment, provide good long-term functional results.
Публикация в New Armenian Medical Journal Vol.9 (2015) Авторы: Шнейдер Ю. А., главный врач ФГБУ "ФЦВМТ" Минздрава России (г. Калининград), Исаян М. В., кардиохирург кардиохирургического отделения №2 ФГБУ "ФЦВМТ" Минздрава России (г. Калининград).